As a GP
I need to know who Advance Decisions are for
So that I know when to recommend one and understand why someone has made one

Just before we all finished up for Christmas (seems a long time ago now) we completed our ‘GP discovery’.
Ten weeks of user research — interviews, desk research and analysis.
We wanted (and are still trying) to figure out if there’s an opportunity for us to better support GPs with Advance Decisions.
This earlier post explains why there is a need to do this. The short version is that the law is good at allowing people to make decisions about their care, but the system lets them down. We now have a better understanding of how and why this is the case.
We chose to speak to 10 GPs. We felt that spending more time with each person and allowing enough time for analysis would be better than cramming in a larger number.
After only a few interviews, we were confident this was the right approach — the detail covered in interviews allowed us to uncover some consistent patterns in behaviour and views.
This research has been eye opening for all of us. Many things we found weren’t necessarily new to us, but hearing things first hand from GPs rather than second hand from patients was hugely revealing.
We now have a much better understanding of the context surrounding the problems we were hearing from people. For example, we now know why some GPs might charge someone for signing their Advance Decision.
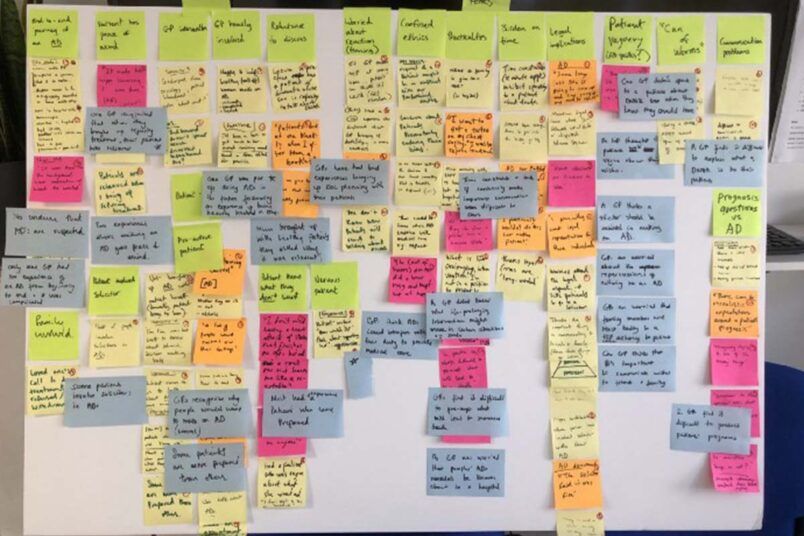
A critical part of the discovery was analysing the interviews and turning all our research from the interviews into ‘user needs’, which are the needs that a user (in our case a GP) has of a service, and which that service must satisfy for the user to get the right outcome for them.
Services designed around users and their needs:
Our analysis generated 20 user needs, categorised into 5 themes:
As a GP
I need to know who Advance Decisions are for
So that I know when to recommend one and understand why someone has made one
As a GP
I need to understand how Advance Decisions benefit people who have lost capacity
So that I can recognise when a patient should make one
As a GP
I need a way to bring death and dying up
So that patients don’t react badly
As a GP
I need to know some patients will find it difficult to raise the idea of refusing treatment
So that I know when to initiate the conversation
As a GP
I need to make talking about death and dying routine
So that I am more comfortable talking about it with every patient
As a GP
I need to know what life prolonging interventions might be given
So that I can explain this to a patient who wants to make an Advance Decision
As a GP
I need to be open to listening to my patients wishes
So that I can understand why they would want to refuse treatment
As a GP
I need to understand my role and responsibility
So that I know what I should do to support people with Advance Decisions
As a GP
I need my patients to clearly explain what they do and do not want
So that I can make sure their Advance Decision is clear
As a GP
I need to know who I can signpost patients to
So that they can be supported with their Advance Decision
As a GP
I need the process to be simple
So that I don’t have to spend too much time on it
As a GP
I need access to an Advance Decision form which I trust
So that I can give it to my patients
As a GP
I need to understand how Advance Decisions fit with my duty to provide medical care
So that I don’t feel conflicted about following an Advance Decision
As a GP
I need to understand why a solicitor doesn’t need to be involved
So that I can advise my patients correctly
As a GP
I need to know more about what an Advance Decision is and the process of making one
So that I understand them
As a GP
I need an easy definition of DNAR
So that I can explain it to my patients
As a GP
I need to know that an Advance Decision is legally binding
So that I feel comfortable and confident following it
As a GP
I need to be aware that my understanding of Advance Decisions might not be correct
So that I proactively look for correct information
As a GP
I need to know that the hospital will know about my patients’ Advance Decision
So that I do not worry that they will be given treatment they do not want
As a GP
I need there to be consistent SNOMED codes
So that I can search for and find a patients’ Advance Decision
A big task for us now is to make these user needs as accessible and useful for our organisation as possible. I’d love to know how other organisations approach this element of a discovery so please get in touch if you have any tips.
At the moment we are discussing ideas for ‘alphas’. Or in non-digital speak, talking about solutions.
We’ve been careful up until now to not jump ahead and think of solutions to problems we heard about in interviews. But now comes the interesting and arguably harder part of making that leap from problem to solution.
For each solution we come up with, we will map it back to the specific user needs we’ve identified. We will also think about costs and feasibility of each.
As a small organisation, we are not blessed with bucketloads of cash and staff available to work on this — so we’ll need to think about impact and reach before committing any resources.
If we decide that there is in fact not much we can do to support GPs with Advance Decisions, we may decide to stop at this point.
If that happens, it might be easy to think it was a waste of time, money and staff time to pursue this line of research. But I think that would be missing the point entirely.
A decision to stop (for the right reasons) would be because lots of research, analysis and frankly hard work has shown that it is the best thing to do.
Regardless of next steps, the findings have prompted some thinking about how we operate and design our services.
It has posed some interesting questions like:
These are big, probing questions to which we need to have answers.
At the very minimum, the 10-weeks of research has resulted in us having to face up to these — for that reason it’s already been worth it.
If you have any thoughts, or would like to be involved with our project then please — get in touch.