
The NHS is in crisis
I want to start talking more about how the crisis in the NHS is starting to feed into our thinking about how we support our service users at Compassion in Dying.
Why? Because I think we have a duty to be honest to people about the barriers they may face. I also think there are some practical things we can do with our content to better prepare people for these interactions.
Crisis? What crisis?
If you watch the news, are on Twitter or have had any sort of interaction with the NHS over the past few years it’s probably safe to say you’ve noticed something is wrong. It’s hard to ignore.
At no other time in the past 50 years have so many parts of the NHS been so close to ceasing to function effectively.
It feels as if everyday there is a story on the news about a new crisis facing the NHS. Whilst I was thinking about this blogpost I even tweeted about how I’d been collecting bookmarks in order to show how bad the situation is.
Here is just a small selection…
- Editorial from BMJ and HSJ — the NHS is not living with covid, it’s dying from it
- British Social Attitudes survey — shows dissatisfaction with the NHS is at the highest levels in 25 years
- BBC News — Cornwall mother, 90, in 40-hour wait for ambulance
- House of Commons health and social care select committee report shows NHS in England facing worst staffing crisis in history
- NHS England data show 24,000 patients were delayed in an Emergency Department for 12-hours or more
I stopped bookmarking after a week — there are only so many ways to say the same thing… the NHS is really struggling.
What does this mean for the people we support?
On many levels, this crisis worries me. It worries me personally — what A+E pressures, and ambulance wait times mean if I or people I care about really need to access these services. But professionally, I worry about what this means for the people we support at Compassion in Dying.
We work in a complex policy area. End of life issues have always felt a bit…behind, or low down on the list of priorities for those at the top.
Yes, there have been positive developments, but it does sometimes feel like an uphill battle to really make sure people are getting the care and treatment they deserve at the end of life.
Before the pandemic, we came across cases where people had poor experiences when trying to get end of life care in line with their wishes. I worry that now, these problems will be worse.
The impact the pandemic has had on staff morale and motivation within the NHS cannot be underestimated. GPs for example seem particularly stretched and under pressure.
For our service users, GPs play an important role. When we help people complete their living will (advance decision), we tell them to share it with their GP.
With most GPs under immense strain — can we reasonably expect them to perform at their best when faced with a person who wants to discuss their end of life wishes? A discussion about someone’s living will can often be a prompt to talk about other things like DNACPR (do not attempt cardiopulmonary resuscitation) forms. How many of these opportunities are being missed?
Of course we should all expect a basic and consistent standard of care — but in the current context can we start to reasonably understand when things go wrong?
It’s starting to become a common theme that people are dropping off their living will forms at reception because they ‘don’t want to bother‘ their GPs. The narrative of busy GPs seems to have already filtered through to the public.
This is quite shocking when you think about it… people are altering their behaviour and interactions with the health system based on their perception of how busy their doctor might be.
The recent results from a British Social Attitudes survey seem to suggest this isn’t a small problem:
This change in behaviour has unintended consequences — we hear for example that peoples’ living wills have been misplaced, or lost when dropped off at GP surgeries.
What can (or should) we do about it?
Above is just one small example of how the NHS crisis can impact our service users. The worrying thing is that we may not really know the full impact of what’s happening to people. Whose job is it to know?
Occasionally I’ll come across a story which puts the crisis into sharp perspective. This tweet did that for me:
This is awful. People are losing hope that the NHS will be there for them when they need it most. Health needs wait for no one, they pay no heed to a system or its intricacies whether it works or not.
As someone who works on our online content, I’m starting to devote more and more headspace to if and how we can better prepare people to interact with an NHS in crisis.
We already do a bit of this, for example in response to the lost forms issue I outlined above — we say to people to check-in with their GP surgery a few weeks after dropping it off to just double check it’s been added to their medical record.
Should we be doing more though? It feels to me there is a new type of content for our service users — it’s not factual information about a topic, but it feels like something we need to highlight…almost a ‘here’s what to expect’ content pattern?
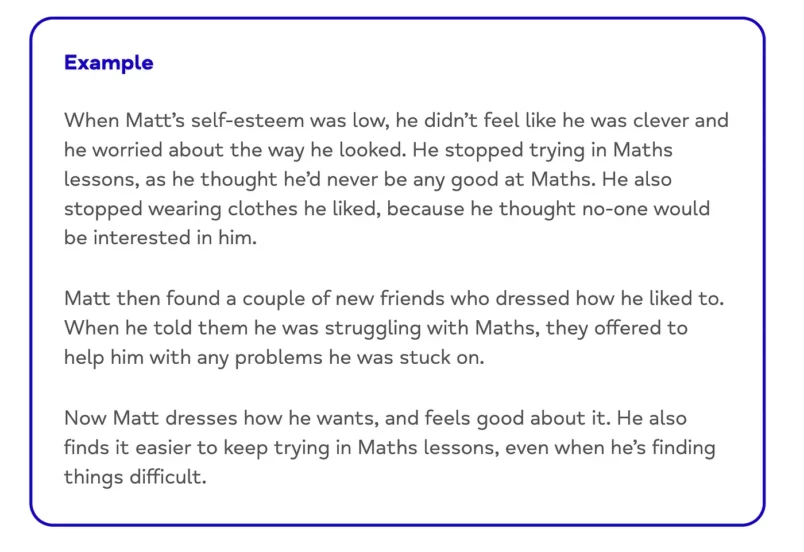
The above example from the Mind website is an interesting content pattern — it’s not quite a case study or quote — it’s different and deliberately so I think.
If we do decide to start weaving in little things like this to better prepare our service users about how the NHS crisis might affect them, then it will be quite a big change.
We need to do some more research into it, but it feels like an ‘organisational need’ to better prepare our service users. Watch this space.
I’d love to have a chat to any other service providers or content designers or anyone really who’s done some thinking on this. Get in touch on Twitter if you want to chat!